Breathing is something we should never have to think about, especially when we are asleep. Yet for people living with sleep apnoea, the night can be filled with interruptions, shallow rest, and exhaustion that lingers well into the day.
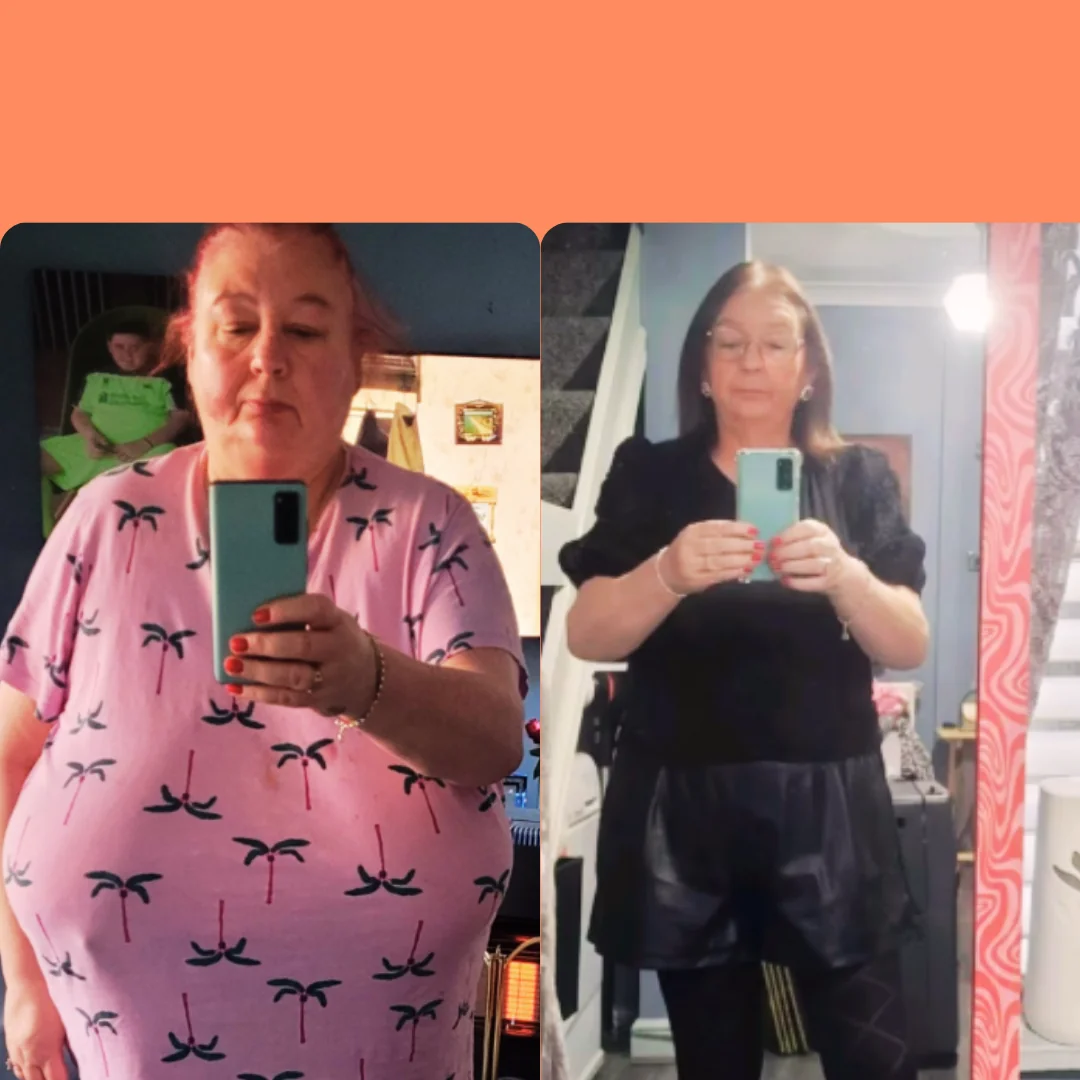
At Phoenix Health, we often hear from patients who say the fatigue and constant tiredness were among the most difficult parts of living with obesity, and one of the most surprising improvements they noticed after bariatric surgery was finally being able to sleep properly again. One of the most common types, obstructive sleep apnoea (OSA), has strong links with obesity. For many patients, bariatric surgery doesn’t just help with weight management; it can also bring relief from the constant struggle to breathe properly at night.
What Is Sleep Apnoea?
Sleep apnoea is a condition where breathing repeatedly pauses and restarts while a person is asleep. In obstructive sleep apnoea, the muscles in the throat relax too much, narrowing or blocking the airway. Oxygen levels fall, the brain senses the problem, and the body briefly wakes just enough to restore breathing. These interruptions are so short that many people don’t even realise they are happening, yet they can occur dozens of times every hour.
The result is a restless night and an exhausted day. People with OSA may wake up with a dry mouth or headache, find it difficult to stay awake during the afternoon, or notice they are never refreshed even after a full night in bed. While loud snoring is often associated with OSA, not everyone who snores has the condition, and not every patient with OSA will snore.
Why Obesity Raises the Risk
Carrying excess weight increases the chances of developing sleep apnoea because fat tissue around the head, neck, and upper body places pressure on the airway. This makes it more likely to collapse during sleep. It’s one of the reasons why people with higher body mass indexes are more vulnerable to the condition.
The impact of untreated OSA is far more serious than poor quality sleep. It can raise blood pressure, increase the risk of heart disease and stroke, worsen type 2 diabetes, and even lead to memory and concentration problems. In some cases, it has been linked to sudden cardiac death. This is why recognising and addressing the problem is so important.
Treatments and Their Challenges
The most common treatment for moderate to severe OSA is the CPAP machine (Continuous Positive Airway Pressure). This device delivers a steady flow of air through a mask to keep the airway open overnight. While highly effective, not everyone finds it easy to use. Some patients feel claustrophobic, find the mask uncomfortable, or simply struggle to adapt.
Other approaches include oral appliances that reposition the jaw, lifestyle changes such as sleeping on your side, cutting down on alcohol before bed, and of course weight loss. These can all help, but for those with severe OSA, they may not be enough on their own.
The Role of Bariatric Surgery in Sleep Apnoea
One of the most significant, yet sometimes overlooked, benefits of bariatric surgery is its effect on sleep apnoea. As weight is lost, pressure on the airway is reduced, making breathing easier during the night. Studies and clinical experience show that around 75%% of patients see their sleep apnoea improve following the bariatric surgery, and many are eventually able to reduce or stop using CPAP altogether.
What’s important to understand is that the improvement is gradual. Patients usually notice changes as the weeks and months go by, but it can take time for the body to adjust fully. Sleep becomes deeper and more restorative as the airway remains open more consistently.
Some patients also report better energy levels and sharper concentration during the day, thanks to improved rest at night. The benefits of bariatric surgery are not limited to sleep alone but extend to heart health, blood pressure and overall wellbeing.
When to Re-Test
If you’ve had bariatric surgery and previously been diagnosed with OSA, it’s worth waiting around six months before arranging a new sleep study. By this point, significant weight loss has usually occurred, giving a more accurate indication of whether the condition has improved or resolved.
Improving sleep apnoea through bariatric surgery highlights just how closely weight and breathing are connected. By reducing pressure on the airway, patients often gain the chance to sleep soundly, wake refreshed, and feel healthier overall. For those who have struggled with restless nights and constant fatigue, the changes can be life-altering. If you’d like to discuss your treatment options, call our clinical team on 01244 738 159 for a free call back.
Medically Reviewed by Lujain Alhassan, BSc, ANutr
Registered Associate Nutritionist and Bariatric Nutrition
References:
Gami, A. S., Olson, E. J., Shen, W. K., et al. (2013). Obstructive sleep apnea and the risk of sudden cardiac death: A longitudinal study of 10,701 adults. Journal of the American College of Cardiology, 62(7), 610–616. https://doi.org/10.1016/j.jacc.2013.04.080
Parish, J. M., & Somers, V. K. (2004). Obstructive sleep apnea and cardiovascular disease. Mayo Clinic Proceedings, 79(8), 1036–1046. https://doi.org/10.4065/79.8.1036
Sarkhosh, K., Switzer, N. J., El-Hadi, M., et al. (2013). The impact of bariatric surgery on obstructive sleep apnea: A systematic review. Obesity Surgery, 23, 414–423. https://doi.org/10.1007/s11695-012-0862-2